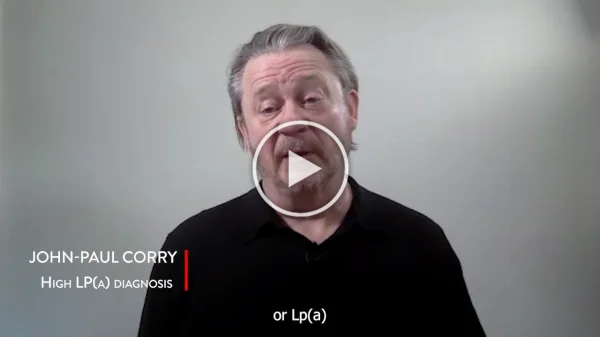
Heart Heroes
Hear from caregivers, cardiologists, patients and their family members – all heroes among us, battling, treating and beating heart disease.
If you’d like to nominate a Heart Hero or are a Heart Hero yourself and would like to share your story, please contact [email protected].








The Heart Hero series consists of personal testimonials that patients, practitioners, caregivers, and others wish to offer and share in their own authentic voice. Any examples of diagnoses, care, treatment, medical processes, or recommendations mentioned in the stories are provided independently of WHF’s policy or scientific and technical outputs.